CORNEAL COLLAGEN CROSS-LINKING FOR KERATOCONUS
Corneal Collagen Cross-linking is an innovative painless therapy developed for treatment of keratoconus, the same therapy is also referred to as CXL, CCL, KXL, CCR or C3-R. Dr. Marco Abbondanza is a leading innovator in this treatment, having pioneered it since 2005 and having introduced it in Italy. Dr. Abbondanza has also been one of the few surgeons that attended official certification courses where the technique was invented, in Dresden, Germany, and Zurich, Switzerland.

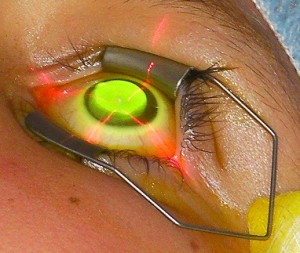
Dr. Marco Abbondanza, MD and eye surgeon, performing Corneal Collagen Cross-linking for keratoconus
Video: Corneal Collagen Cross-linking for keratoconus
The normal cornea consists of numerous layers of collagen fibers, approximately 350 layers in an average thickness of 520nm, with molecular links between the adjacent layers which are known as crosslinks. These crosslinks are responsible for the toughness and elasticity of the normal cornea. In corneas affected with keratoconus the corneal links are reduced and the cornea loses its natural resistance. The aim of the treatment is to increase the strength and durability of the cornea by stimulating and thus increasing the number of corneal crosslinks between the adjacent collagen layers within the cornea.
The procedure was first developed in Germany and clinical trials have been in course since the year 1998, in Italy Corneal Collagen Cross-linking is performed since 2005, when introduced by Dr. Abbondanza.
 The technique is essentially quite simple. An eye drop that consists of a solution containing riboflavin is applied to the eye and a carefully dosed quantity of UVA radiation is applied to the eye over a five minute period, the procedure is repeated 6 times for a total of 30 minutes of UVA exposition. In the first trials the treatment was performed in eyes with initial keratoconus. The treatment aimed to increase corneal resistance, and thus, to essentially prevent evolution of keratoconus.
The technique is essentially quite simple. An eye drop that consists of a solution containing riboflavin is applied to the eye and a carefully dosed quantity of UVA radiation is applied to the eye over a five minute period, the procedure is repeated 6 times for a total of 30 minutes of UVA exposition. In the first trials the treatment was performed in eyes with initial keratoconus. The treatment aimed to increase corneal resistance, and thus, to essentially prevent evolution of keratoconus.
The excellent results following these initial cases of treatment allowed the extension of the treatment to eyes presenting different stages of keratoconus. The extent to which corneal cross linking is beneficial in different stages of keratoconus is dependent on a number factors, such as corneal thickness and the rate of evolution of the disease. Dr. Abbondanza performs Corneal Collagen Cross-linking alone, or associated with Mini Asymmetric Radial Keratotomy (MARK), microsurgical technique he conceived in 1993. An important research, published in 2019, confirms the validity of the MARK + CXL combined intervention, as it is able to halt the progression of keratoconus while improving visual acuity. Such results were recorded and evaluated with long-term follow-up (click here to read the research). Another clinical study, published in 2016 by scientific journal Acta Medica International (click here to read it), showed that Dr. Abbondanza’s MARK+CXL combined protocol, knows as the “Rome Protocol”, produces an average reduction in corneal curvature of 3,7D and a significant decrease of corneal aberrations, along with the halting of the disease itself.
Patients that are considered for treatment, must undergo an extensive clinical workup including computerized corneal tomography, corneal topography, endothelial microscopy, ultrasound pachymetry, b-scan sonography, keratometry and biomicroscopy. The most important clinical parameter that must be considered before treatment is corneal thickness, in fact, the cornea and also the riboflavin solution act as a filter to UVA radiation. If the cornea is not sufficiently thick, necessary measures must be taken to reduce UVA 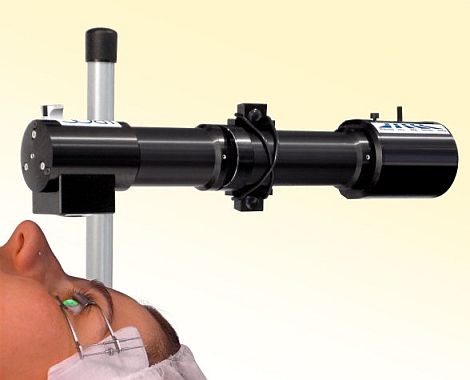 penetration to the eye, such as placement of a corneal contact lens during treatment.
penetration to the eye, such as placement of a corneal contact lens during treatment.
The possibility of associating MARK and Corneal Collagen Cross-linking offers the possibility to increase both visual acuity and corneal strength in many patients, in fact MARK has potential to increase visual acuity considerably in selected patients with keratoconus.
The ultimate goal in these conservative treatments for keratoconus patients is to postpone or possibly eliminate the necessity of penetrating keratoplasty, and to improve the quality of vision of patients as long as possible.
Technically, corneal crosslinking may be performed in two ways. The first consists in removing the most superficial layer of cells of the corneal epithelium before treatment. This technique guarantees the most complete absorption of the riboflavin solution into the corneal stroma, but the corneal epithelial removal may cause discomfort following treatment. This discomfort is very variable in patients and ranges from mild to moderate and is usually limited to the first 2 days following treatment, although a mild irritation may persist for a week until the epithelial layer of the cornea reforms. The symptoms are perfectly controllable by using analgesics, local non steroidal anti inflammatory treatment (FANS), and lachrymal substitutes associated with the placement of a corneal contact lens for the few days following treatment.
The second technique that is preferred by some Authors reduces patient postoperative discomfort by leaving the corneal epithelium in place, these Authors recommend application of riboflavin for a longer period to allow more time for absorption of the medication before the actual UVA application.
In conclusion, crosslinking is a very effective technique and offers a unique possibility to strengthen the cornea in patients with keratoconus. As with all medical procedures a complete pre-treatment individual ophthalmologic clinical examination is necessary to evaluate the opportunity for treatment.
The results achieved by ophthalmologists all over the world performing Crosslinking have proved an enduring stability and thickness of the cornea after treatment, as well as a marginal improvement of visual acuity, as demonstrated by Dr. Abbondanza scientific study (click here to read the full study published by a leading international journal).
.
